Tuesday, March 23, 2010
Asthma Management Plan and Prognosis
· A written asthma action plan detailing for the individual patient the daily management (medications and environmental control strategies) and how to recognize and handle worsening asthma
· Particularly recommended for patients who have moderate or severe asthma, a history of severe exacerbations, or poorly controlled asthma
· The written asthma action plan can be either symptom or peak-flow based; evidence shows similar benefits for each
· Developed jointly between the healthcare advisor and the patient
· There are many different asthma management plan formats. However, all action plans must have the following components:
o Recommended doses and frequencies of daily medications
o How to adjust medicines at home in response to particular signs, symptoms and peak flow measurements
o Listing of the patient’s peak expiratory flow (PEF) levels, including personal best PEF and calculated PEF zones based on personal best. PEF monitoring recommended for moderate and severe asthma only
o Symptoms indicating the need for closer monitoring or acute care
o Emergency telephone doctor, emergency department, rapid transportation and family/friends for support
o A list of triggers that may cause an asthma attack to inform the patient and others on what triggers to avoid
· A copy of patient’s asthma action plan should be:
o Carried with the patient
o Kept in the patient’s medical chart
o Provided to the patient’s day care, school or worksite
o Provided to the patient’s coach/physical education teacher
o Provided to other contacts of the patient as needed
Symptom-Based Plan
Ø Band 1
o Taking reliever medications not more than 3-4 times a week
o Free of regular night-time wheeze, cough or chest tightness
o Able to take part in normal physical activity without getting asthma symptoms
o Means there is no need to adjust medication
Ø Band 2
o Require reliever medication more than once a day
o Asthma status is deteriorating
o Amount of medication should be doubled
Ø Band 3
o Need short-acting reliever medication every 3-4 days
o Dangerous situation and need medical attention urgently
o Need to start or resume oral steroid treatment and contact doctor ASAP
Ø Band 4
o No relief with bronchodilators
o Emergency situation where situation gets worse very quickly
o Need an ambulance and continue use of bronchodilators
Peak-Flow Based Plan
Ø Objective measure of asthma severity in people with moderate to chronic asthma
Ø Little evidence showing that it is better than a symptom based plan
Ø Peak flows are not 100% accurate
Ø Sometimes, they overestimate the need for drugs, while in other cases they fail to diagnose an asthma attack
Ø Readings can be incorrect because of wrong technique
Ø Technique of using a peak flow meter:
o Sit upright/stand up straight.
o Slide a marker to the end.
o Hold the meter horizontal.
o Keep your fingers away from the marker. Take a deep breath.
o Put the meter in your mouth. Close your lips around the mouthpiece and blow out as hard and as fast as you can.
o Repeat the entire routine three times.
o Take note of your highest reading.
o Keep a chart of your peak flow rate – upon rising in the morning and early in the evening.
o Important to use the peak flow meter at the same time everyday
Ø A personal best peak flow is obtained by keeping the records for a few days and determining what is normal for you.
Management of Catastrophic Sudden Severe (Brittle) Asthma
ª Unusual variant of asthma in which patients are at risk from sudden death despite the fact that their asthma may be well-controlled between attacks
ª Severe life-threatening attacks may occur within hours or even minutes
ª These patients require:
§ Emergency supplies of medications at home, in the car and at work
§ Oxygen and resuscitation equipment at home and at work
§ Nebulized β agonists at home and at work
§ Self-injectable epinephrine (adrenaline): 2 Epipens of 0.3 mg epinephrine at home, at work and to be carried by the patients at all times
§ Prednisolone 60 mg
§ Medic Alert bracelet
ª On developing wheeze, patient should attend the nearest hospital immediately
Prognosis for Asthma
v Is chronic, although may go into long periods of remission
v In mild to moderate cases, asthma can improve over time and many adults even become symptom-free
v Even in some severe cases, adults may experience improvement depending on the degree of obstruction in the lungs and the timeliness and effectiveness of the treatment
v However, although asthma often improves in children as they reach their teens, it is now realized that the disease frequently returns in the second, third and fourth decades
v In about 10% of the severe persistent cases, airways remodelling lead to progressive and irreversible problems in lung function, even in aggressively treated patients
v Led to reappraisal of the treatment strategy for asthma, mandating the early use of controller drugs and environmental measures from the time asthma is first diagnosed
v Death from asthma is a relatively uncommon event especially for a person receiving proper treatment
Saturday, March 6, 2010
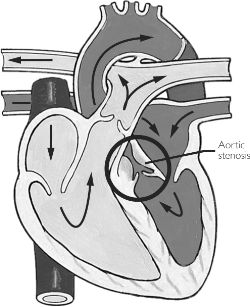
Echocardiography (Non-invasive diagnostic technique)
1. The evaluation of cardiac structure and function with images and recordings produced by ultrasound
2. There are many echocardiographic modalities:
- M-mode
- 2D
- 3D
- Doppler
3. Echocardiographic findings in aortic stenosis case:
a. 2D echocardiographer
- Thickened Aortic Valve Leaflets

- leaflet is more reflective and can be seen in systole and diastole
- best visualized in 2D
- right coronary cusp most affected
- left coronary cusp least affected
- Restricted Leaflet Motion
- systolic separation of right coronary cusp (anterior) and noncoronary cusp (posterior) falls below 1.5 cm in adults
- fused commissures results in systolic doming of the valve
- Narrowed orifice
- acquired - advanced valvular obstruction with calcification
- congenital – unicuspid or bicuspid aortic valve with/without calcification
 b. M-mode (Not reliable technique for assessing the severity of aortic stenosis)
|
Doppler (Very reliable)
c. Spectral Doppler (Very reliable)
- Increased Peak systolic velocity (more than 3.5 m/sec)
- Peak systolic velocity ranged from 1.2 to 3.3 cm/s, and peak diastolic velocity ranged from 1.6 to 4.5 cm/s (http://www.ajnr.org/cgi/content/abstract/24/2/169)
- Increased Pressure Gradient (Bernoulli). Bernoulli principle can be used to calculate AVA
- Decreased Valve Orifice
d. Color Flow Doppler
- Use one color for blood flowing towards the transducer and another color for blood flowing away
- High velocity systolic jet
* Transesophageal echo/Doppler ultrasound and transthoracic technique are very useful
Cardiac catheterization
- Introduce a thin radio-opaque tube (catheter) into the circulation
- Used to record the systolic pressure difference (gradient) between the aorta and the left ventricle and assess left ventricular function
- This is done by measuring simultaneous LV and ascending aortic pressures and measuring cardiac output
- Data that can be obtained:
a. Left ventricular pressure
- Elevated because the ventricle has to force blood through the narrowed opening of the aortic valve
- Elevated end diastolic pressure occur as ventricle adapts to the pressure overload condition
b. Left atrial pressure
- Increase as atrium adapts to changes in left ventricular pressures
c. Aortic Valve Gradient
Provocative Diagnostic Test
1. As mentioned above, the severity of AS may be in doubt due to small mean aortic valve gradient. The calculated AVA can be small because of severe stenosis or small stroke volume.
2. In this test, an inotropic agent such as dobutamine, which will cause an increase in cardiac output (stroke volume) and heart rate (shortening of systolic ejection time), will be used.
3. Then, measure cardiac output and LV and aortic pressures simultaneously, both before and during dobutamine infusion because it will cause systemic vascular resistance either increase or decrease.
4. Whether the AS is mild or severe, the gradient increases with dobutamine infusion.
Gated Blood Pool Radionuclide Scans
1. It uses radioisotope dye that shows how blood pools in the heart during rest, exercise, or both. It gives information on how well the heart is pumping blood and if it is working harder to make up for one or more blocked arteries.
2. It can also find ejection fraction, which is the percentage of blood that is pumped out of the heart’s left ventricle.
3. A radioactive substance is injected into the bloodstream. The radioactive substance tags or labels the red blood cells in the blood. This substance is safe and will not cause any harm. A gamma-ray camera is used to take pictures of the heart as the tagged red blood cells circulate.
Exercise testing
1. It is not safe in symptomatic patients with severe AS. Hence, it is only best to use for asymptomatic patient. Indeed, patients with severe AS need to undergo aortic valve replacement (AVR).
2. In the absence of coronary disease, most patients with severe AS exhibit a normal cardiac output at rest. However, the hypertrophic left ventricle is less compliant than normal and LV end-diastolic pressure is often increased.
3. During exercise, cardiac output fails to increase normally in most of patients with severe AS.
4. The mechanical obstruction to blood flow posed by the stenotic valve limits blood flow and the reduced diastolic compliance of the hyperthrophied ventricle contributes by reducing the potential to augment end-diastolic volume and utilize the Frank Starling mechanism during exercise. As a result, stroke volume fails to rise and changes in cardiac output largely depend on changes in heart rate.
5. Blood pressure normally increases during exercise, but inadequate cardiac output or abnormal peripheral vascular response can result in hypotension.
6. Arterial and venous vasodilatation with bradycardia, mediated by sudden changes in LV pressure and baroreceptor activity (the Bezold Jarish reflex), play a role in effort-related hypotension and syncope in patients with AS.
7. Basically, exercise testing can only give prognostic information. Hence, it can be used to provide an exercise prescription and to reassure the patient who might otherwise excessively limit his or her activity.
Clinical Decision Making
It includes a complete clinical evaluation:
1. History
2. Physical examination
3. ECG
4. Chest Radiography
5. Disease of all cardiac valves, ventricular function, hemodynamic effects, as well as CAD, other cardiovascular disease, and disease of other organs, should be diagnosed and the severity assessed
6. Additional testing
Clincial examination
1. For a complete physical examination, it was presented by Joanna last week. Hence, I will focus on auscultation and pulse which is very important in diagnosing AS.
Pulse
1. The arterial pulse rises slowly, taking a longer time than normal to reach peak pressure, and the peak is reduced (parvus et tardus). Parvus et tardus pulse means an arterial pulse that is small and has a delayed systolic peak (severe AS often have it). It is easier to detect in the carotid artery than in more distal arteries.
2. The pulse pressure may be narrowed. The anacrotic notch on the upstroke is best appreciated in the carotid arteries. The more severe the valve stenosis, the lower the anacrotic notch on the arterial pulse. Anacrotic means a detectable shoulder on the upstroke of the carotid pulse. Palpable coarse vibrations often are present as a systolic thrill over the slowly rising carotid pulse.
3. Uncomplicated severe AS will have a parvus et tardus pulse but can also occur in relatively mild stenosis.
4. The JVP is normal unless there is heart failure.
Auscultation
1. There may be a palpable fourth heart sound (S4). There is S4 gallop sound, a midsystolic ejection murmur that peaks late in systole and a single second heart sound (S2) because A2 and P2 are superimposed or A2 is absent or soft.
2. There is often a faint early diastolic murmur of minimal aortic regurgitation (AR).
3. In the young patient with AS, a systolic ejection sound (systolic ejection click) initiates the systolic murmur but later tends to disappear as AS becomes severe.
References:
1. Kumar & Clarks Clinical Medicine 7th Edition 2009, Aortic Stenosis (pg. 765), Kumar, P. & Clark, M. (eds.), Saunders Elsevier, London.
2. Rahimtoola Shahbudin H, "Chapter 75. Aortic Valve Disease " (Chapter). Fuster V, O’Rourke RA, Walsh RA, Poole-Wilson P, Eds. King SB, Roberts R, Nash IS, Prystowsky EN, Assoc. Eds.: Hurst's The Heart, 12e: http://www.accessmedicine.com.ezproxy.lib.monash.edu.au/content.aspx?aID=3062773
3. http://www.echo-web.com/asp/samples/sample5.asp
4. http://resources.metapress.com/pdf-preview.axd?code=5v4t3r760358h403&size=largest
5. http://www.ajnr.org/cgi/content/abstract/24/2/169
Friday, March 5, 2010
Treatment and Management for Aortic Stenosis
SURGICAL
Harden valves by calcification and deformities should undergo surgery.
Note: Valve replacement is necessary for all symptomatic patients.
This is because prognosis of patients with onset syncope, angina or heart failure due to aortic stenosis is poor, about 50% 3-year mortality rate.
Aortic Valve Replacement
3 types
1. Mechanical
Pros
-Most durable
- Recommended for 60 y.o and below
- anticoagulation can be accomplished at lower risk
Cons
-Need of anticoagulants-- Thromboembolic complications possible in the absence of anticoagulation include stroke and fixation of the valve in either the open or closed position.
Type of valve:
Caged-ball and tilting-disk valves were popular in the twentieth century, the bileaflet valves are most commonly used today.
2. Pulmonic valve transplantation (Ross Procedure)
- patient's native pulmonic valve (autograft) is removed and sewn into the aortic position.
-prosthetic valve or a pulmonic homograft is then sewn into the pulmonic position.
Pros:
- Own biological valves has excellent hemodynamic characteristics, plus durability esp during high pressure, high stress and when left sided circuit where prostheses can fail.
- Low stress on pulmonary valves as it is low pressure and low stress, it is better to place the bioprosthesis here rather than the aortic valve position.
Cons:
-Amount of surgery is very demanding and tedious procedures.
3. Bioprostheses
2 types:
Heterographs
- From porcine aortic valve leaflets or bovine pericardium (both preserved with glutaraldehyde).
- Advantage: low thromboembolic potential. In the absence of atrial fibrillation, the risk of thromboembolism following aortic valve bioprosthetic implantation is less than 1 event per 100 patient years, and anticoagulation is not required.
- Also if the patient is of normal sinus rhythm, anticoagulants are not needed.
- Disadvantage: If AS is accompanied with AF, risk of thromboembolism
: Durability low (approximately 50% of valves have failed within 15
Years.
: Calcification and degeneration of the valves leads to tears in the cusps or stenosis of the valve or flail leaflets.
: modest obstruction to outflow and a residual pressure gradient in patients requiring implantation of small valves.
Ideal Patients for heterographs: elderly patient whose life expectancy is less than the durability span of the valve or the patient for whom anticoagulation poses a significant risk.( above 65 y.o)
Homographs
- harvested from human donors.
- Pros: excellent hemodynamic profile
o relatively resistant to bacterial endocarditis
o more durable than heterograft valves
- Cons: use of homograft valves is limited by availability-- many potential donors for homograft valves are also whole-heart donors, the number of available homografts is small.
-Ideal for: patients with a small aortic root where other types of prostheses might cause a transvalvular gradient.
Alternative for surgery is
1. Balloon Dilatation ( Valvuloplasty)
Procedure: a thin tube (catheter) with a small deflated balloon at its tip (balloon-tipped catheter) is inserted through the skin in the groin area into a blood vessel, and then is threaded up to the opening of the narrowed heart valve. The balloon is inflated to stretch the valve open and relieve the valve obstruction.
4 hour procedure
Patient placed supine on the x-ray table
Upper leg is washed and treated with iodine to prepare for insertion of catheter.
Under local anesthesia, the cardiologist inserts the catheter to the blood vessel, which passes the smaller balloon tipped catheter through the first catheter.
Guided with an x-ray monitor, visualization of the catheter in the blood vessel can be monitored as it progressively enters the coronary artery in the heart.
The deflated blood vessel is placed at the opening of the valve and then inflated repeatedly to allow the pressure to dilate the valve.
This is done by splitting the valve leaflets apart.
Once widened, the balloon tipped catheter is removed.
The other catheter must remain in place for 6 to 12 hours because the procedure must be repeated.
2x ballon valvuloplasty is performed in high risk patients (elderly) as this is more efficient in restoring blood flow.
PHARMACOLOGICAL
Antibiotic prophylaxis
- infective Endocarditis
High risk infection in mitral valve prolapsed
High risk infection in valve replacement (accompaniment with aortic valve replacement)
High risk in thickened valve leaflets
Moderate risk in acquired valvular heart disease
Moderate risk in structural cardiac abnormalities
Drug Regimen (Note: For adults!)
Amoxicillin (beta lactam antibiotic, moderate spectrum, target cell wall for both gram negative and gram positive bacteria)= 3g oral 1 hour preprocedure or 2g IV <30>70
Weight < 50kg
Liver Failure
Recent history of bleeding
Recent surgery
International normalized ratio (INR): the ratio of the time taken for a patient's blood to clot compared with a normal person not taking warfarin. Thus a normal person will have an INR of 1.
INR should be maintained between 2.0 and 2.5
At the induction phase, monitoring of 1-3 days should be observed, until the INR target value is consecutive for 2 measurements.
After that, monitoring every 2-3 times a week is needed.
Note: Warfarin also can be used as a means of prevention of recurrent transient ischemic attacks
Contraindications of warfarin related to heart:
If the patient has subacute endocarditis, warfarin will cause hemorrhaging.
Also, pericarditis and pericardium effusion also is a contraindication of using warfarin
http://www.ohsu.edu/academic/medicine/residency//handouts/pharmpearls/General%20Care/WarfarinProtocol.pdf.
http://www.accessmedicine.com.ezproxy.lib.monash.edu.au/content.aspx?aID=3250101&searchStr=aortic+valve+stenosis
http://www.surgeryencyclopedia.com/A-Ce/Balloon-Valvuloplasty.html
http://www.accessmedicine.com.ezproxy.lib.monash.edu.au/content.aspx?aID=3646902&searchStr=aortic+valve+replacement#3646902
K. Parven & C. Michael (eds.) 2009, Kumar & Clark's Clinical Medicine Seventh Edition.
Possible DDx for AS
1. Mitral regurgitation
- This is a condition where mitral valve allows part of left ventricular stroke volume to regurgitate into the left atrium, imposing load on both ventricle and atrium. Usually, holosystolic, soft murmur is heard when auscultated at the apex together with radiation to the left axilla, medium to high pitch with a blowing quality. In posterior cusps disorder of mitral valve results murmur that is radiating towards sterna border rather than the apex, increased intensity through the duration of systole and peaks late during systole.
2. Hypertrophic obstructive cardiomyopathy

-Also known as idiopathic hyperthropic subaortic stenosis (IHSS) where there is thickening of the myocardium which reduce blood flow from the heart thus decreasing cardiac output. The standing and the strain phase of Valsalva can increase the intensity of HOCM murmur and mimic a murmur consistent with AS. IHSS is ruled out from AS by the diminished systolic murmur with squatting and the biphasic pulse.

3. Supravalvular aortic stenosis
-A condition where the ascending aorta beyond the superior margin of the sinuses of Valsalva is narrowed and leads to LV hypertrophy. Patients may show up with dyspnea on exertion, angina and syncope. Upon auscultation, murmur is crescendo-decrescendo in shape, low pitched and best heard at the base of the heart where the site is higher in valvular aortic stenosis. The findings that rule out Suprevalvular aortic stenosis is the absence of ejection click and cineangiography.
4. Congenital subvalvular aortic stenosis
-The physical findings in this condition shows major resemblance to those with AS except the initiation of aortic valve closure from the increased level of aortic pressure proximal to stenotic area, sporadic systolic ejection sound, transmission of a thrill and murmur to the neck. In physical examination, patients reveals higher systolic pressure in right arm than the left because of the selective streaming of blood into the innominate artery.
5. Ventricular Septal Defect (VSD)
-This condition can be either congenital or acquired following episodes of MI. VSD murmur can present depending on how severe the defect is and also the pressure difference between right and left ventricles. Holosystolic or crescendo-decrescendo murmur maybe heard during auscultation in VSD which mimics AS murmur. Echocardiography is widely used to differentiate VSD from AS.

6.Aortic sclerosis
-Results from degeneration and calcification of the aortic cusps, predominantly at their base. This abnormality produces a peaked midsystolic murmur, accompanied by a normal second heart sound and carotid pulse upstroke that is identical in character to aortic valvular stenosis. The responses to physiologic and pharmacologic interventions are identical to those of functional systolic ejection murmurs. Echocardiographic studies suggest that aortic sclerosis is common in the elderly and may be the single most common cause of systolic murmur in this population.
Causes of systolic heart murmur
-valvular aortic stenosis
-aortic sclerosis
-supravalvular aortic stenosis
-subvalvular aortic stenosis
-hypertrophic obstructive cardiomyopathy
-valvular pulmonic stenosis
-pulmonary infundibular stenosis
-atrial septal defect
-tetralogy of Fallot
Causes of chest pain
Angina
MI
Pleuritic pain
Cervical or upper thoracic spine disease
Dissecting aneurysm
Massive pulmonary embolism
Spontaneous pneumothorax
Gastro-oesophageal reflux
Cholescystitis
Virus (eg, Coxsackie B infection, HZV)
Reference List
-Tally and O'Connor. Clinical Examination: a systematic guide to physical diagnosis.
-http://www.fpnotebook.com/cv/valve/artcstns.htm
-www.acponline.org/essentials.
-K. Parven & C. Michael (eds.) 2009, Kumar & Clark's Clinical Medicine Seventh Edition
-Lim, E Loke, YK & Thompson, A 2007. Medicine and Surgery an Integrated Textbook, Elsevier Limited.
-http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=cm&part=A746

